Preparation for Semen Analysis (Seminal Fluid Analysis – SFA) can be exhausting since there are multiple principles you should follow in preparation, collection and transportation of semen to the laboratory.
Should you really bother about the Semen Analysis Preparation?
33% is a magical number in the statistics related to infertility.
- 33% of all the cases of infertility are due to male factors
- 33% of all the infertility cases are due to female factors
- The remaining 33% of the cases are due to mixed causes.
Right! So, if the causes are equally distributed among men and women, whom should be investigated first? Of course it depends. But Doctors often prefer to test the man first because of several reasons.
- Semen analysis is cheaper than female investigations.
- Seminal Fluid Analysis is highly sensitive to male infertility.
- Male infertility is easier to treat than most female causes.
The bottom line is, Semen Analysis is a cheaper, accurate and better than most tests for female causes of infertility. If the male defects are identified by Seminal Fluid analysis (SFA) you don’t have to pay for expensive investigations for female causes.
But there’s one problem with Seminal Fluid Analysis. The sperm counts tend to vary from one day to the next. The best way to tackle this is a good preparation. Learn how to prepare better for the Semen Analysis to get the most accurate results.
Semen Analysis Preparation
Before the Collection
- Your doctor (and laboratory technicians) will advise you on the preparation, collection and transportation of semen samples. Make use of this opportunity to clear any doubts you have regarding preparation, collection or transportation.
- Refrain from Masturbation or Intercourse (complete abstinence) for a minimum of 2 days or a maximum of 7 days.
- An abstinence period of at least 2 days helps to develop a good sperm count and it also permits the existing sperms to mature.
- But longer periods of abstinence may subject the sperms to deteriorate with aging (senescence)
- An abstinence period of 3-5 days is considered ideal.
- Avoid caffeine, alcohol, tobacco, recreational drugs and other medications as instructed by the Doctor.
Note: Cimetidine (H2 receptor blocker), is a drug used to treat Peptic Ulcer Disease and Gastro Oesophageal Reflux Disease. It is known to affect the sperm concentration. But the sperm motility and morphology are not affected.
During the Collection
- Collect the Sample in a Private room close to the laboratory or at the clinic.
- The sample should be brought to the Laboratory within 30 minutes to 1 hour after the ejaculation.
- It also helps to minimize the temperature fluctuations during the transportation.
- Use the special container you received from the laboratory, to collect the Sample.
- The container should be a clean, wide-mouthed and made of glass or plastic.
- The container should have been confirmed to be non-toxic for sperms.
- Label the container with your name, Date of Birth and Time of Ejaculation.
- Follow aseptic techniques to prevent contamination of commensals (friendly organisms from the skin)
- You should start with passing urine.
- Wash your hands and penis with soap
- Rinse away the soap thoroughly.
- Dry hands and penis with a clean disposable towel.
- Don’t use any lubricants (they interfere with sperm motility)
- Ejaculate into a sterile container
- The sample should be collected by Ejaculation into the above container.
- Semen sample should be complete. There shouldn’t be any loss of even a fraction of semen. (You have to report any loss of any fraction of semen)
During the Transportation of the Sample
- Bring the sample to the laboratory within 30 minutes to 1 hour after the ejaculation. (It should be analysed in the laboratory within 1 hour after the ejaculation)
- You will have to maintain the sample temperature between 20 °C and 37 °C, during the transportation.
Note: Don’t store the semen sample in a refrigerator. The Low temperatures will affect the viability and motility of sperm cells.
Can you collect Semen at Home?
Collection of semen at home is allowed in special circumstances like a demonstrated inability to ejaculate by masturbation at the clinic or lack of adequate residence facilities close to the laboratory.
You will receive clear written and verbal instructions regarding collection and transportation of the sample. And you should report if the sample if complete or if there’s any loss of any fraction of the sample.
The laboratory will also provide you a pre-weighed container with your name and identification number on the label.
You should record the time of semen collection and deliver the sample to the laboratory within 30 minutes to 1 hour of collection.
You will have to maintain the sample temperature between 20 °C and 37 °C, during the transportation.
Can I collect Semen by a condom?
Collection by a condom is allowed in special circumstances like demonstrated inability produce semen by masturbation.
You should use only nontoxic condoms specially designed for sperm collections. There are available in the commercial market.
You should record the time of semen collection and deliver the sample to the laboratory within 1 hour of collection.
You will have to maintain the sample temperature between 20 °C and 37 °C, during the transportation.
Note: Ordinary Latex condoms have special chemical agents to interfere with the sperm motility. Therefore they should be avoided when you are collecting a sample for Semen Analysis.
Can I use Coitus interruptus for Sperm Collection?
The simple answer is no. The first portion of the sperm sample contains the majority of sperm cells. They may be lost during Coitus Interruptus.
The sample will also be contaminated with the micro-organisms in the female genital tract.
The acidity in the Female reproductive tract will lower the sperm motility.
What if I failed Semen analysis preparation, collection or transportation of Semen sample?
Then you have to inform the laboratory and recollect the samples again after 2-7 days of abstinence.
How the Seminal Fluid Analysis is conducted and what are the normal values?
- The initial Macroscopic Examination
- Preferably at 30 minutes, but no longer than 1 hour after ejaculation
- The following features are examined with macroscopically
- Semen Viscosity: High viscous seminal fluid will restrict the sperm motility. It could also be due to high antibody coated sperm cells.
- Semen Appearance: The normal semen is grey-opalescent. Reddish sample could indicate the presence of Red blood cells. A yellowish sample could indicate Jaundice, or taking certain drugs or vitamins.
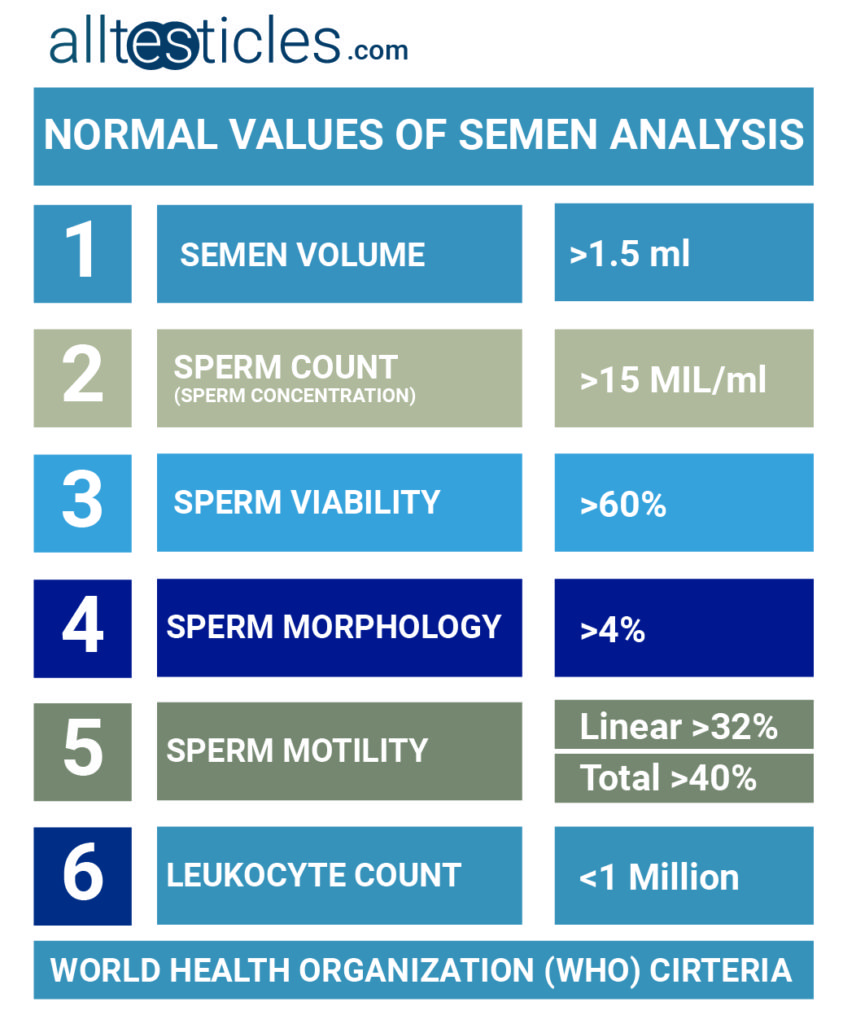
- Semen Volume: Normal Semen Volume should be more than 1.5 ml
- Semen Ph.: Normal Seminal Ph. value is between 6 and 10. Acidic Ph. values can interfere the sperm motility and could indicate the presence of an infection in the male reproductive tract.
- Initial Microscopic Examination
- Preferably before 3 hours after the Ejaculation.
- The following features are examined microscopically.
- Sperm Morphology (Sperm shape): at least 4% of all sperm cells should have the normal shape form.
- Presence of White or Red Blood Cells: Should be minimal
- Sperm Motility (swimming ability)
- Categories of sperm movement
- Progressive (Linear) motility: at least 32% of all sperms should show progressive motility. This is the best indicator of sperm motility.
- Non Progressive motility: Moving in circles without making any progression towards the egg in the female fallopian tubes.
- Total motility: The sum of progressive and non-progressive motility
- Should be at least 40%.
- This measurement is considered, when the progressive motility is less than 32%.
- Immobility: No movement at all
- Categories of sperm movement
- Sperm Vitality
- It is estimated by assessing the membrane integrity of sperm cells. The ideal vitality (viability) should be more than 60% in a normal person.
- Sperm Concentration (Sperm Count)
- Should be more than 15 million/ml in a normal semen sample.
What if the Semen Analysis Report is abnormal?
Don’t worry yet. The sperm quantity and quality varies from one day to the next. Even if your semen analysis preparation is 100% according to the instructions, there’s still a chance for your report to be abnormal because of this variations. For that reason, when one analysis report is abnormal, doctors instruct you to repeat the test after another 3 months. Two abnormal reports 3 months apart, probably suggest that you have an underlying cause of male infertility.
Summary
- Seminal Fluid Analysis is cheaper and more accurate than investigations carried out to identify causes of female infertility.
- Semen Analysis is affected by a number of external and internal factors.
- An adequate preparation is vital for the success of the Seminal Fluid analysis.
- An abstinence period of 2-7 days required during the semen analysis preparation.
- Seminal Fluid analysis should ideally be done at the laboratory or at a facility close to the laboratory, with aseptic techniques without using sperm-toxic agents.
- The semen samples should be transported to the laboratory within 1 hour.
- Seminal Fluid analysis can identify the abnormalities in sperm shape, motility, viability and concentration.
- One abnormal Seminal Fluid Analysis report is not sufficient to diagnose male sub-fertility. A person should repeat the Semen analysis again in 3 months again.
Source:https://www.who.int/reproductivehealth/publications/infertility/9789241547789/en/